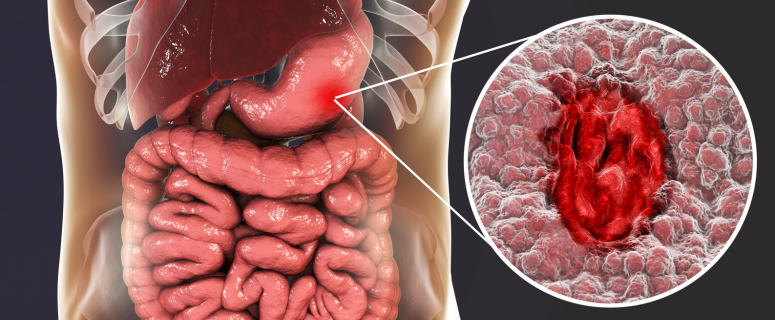
Food plays the most critical role in a healthy lifestyle. A good diet is crucial to maintain your body’s functioning. But, sometimes, you can’t eat food according to your taste due to some health problem, and individuals with Ulcerative Colitis, often known as UC, usually suffer from this situation. UC is an Inflammatory bowel disease (IBD) that affects your large intestine and rectum. You can feel a disturbance in your digestive tract after having a meal. So, having an anti-inflammatory diet plan is a must for people with ulcerative colitis. Yet, a balanced diet can help you reduce Ulcerative Colitis symptoms. People with UC need a meal plan with trigger foods like fiber-rich foods, lean proteins, and healthy fats. In this article, we have prepared a 7-day meal plan for ulcerative colitis to ensure you can intake the right foods in the correct quantity.
7-Day Meal Plan For Ulcerative Colitis and Crohn’s Disease
Here is the 7-day meal plan for people with Ulcerative Colitis (UC).
1: Setting the Tone for a Gut-Friendly Week
- Breakfast: Microwaved old-fashioned oats with lactose-free milk, cinnamon, and cooked diced apples.
- Lunch: Baked chicken seasoned with your favorite spices, served with roasted carrots drizzled with olive oil and steamed rice.
- Dinner: Baked salmon seasoned with lemon juice, garlic, and pepper and served with peeled and baked summer squash and green beans seasoned with olive oil, garlic, and pepper.
- Snacks: A small tuna packet, peaches canned in water or juice, applesauce, and a hard-boiled egg.
2: Adding Wholesome Grains and Lean Proteins
- Breakfast: Plain, lactose-free, nonfat Greek yogurt topped with melted, creamy nut butter. Add fresh-squeezed fruit and vegetable juice.
- Lunch: Leftover cooked salmon served cold with reheated sweet potatoes and green beans.
- Dinner: Harvest soup made with pureed, roasted red peppers, sweet potatoes, apples, and carrots, served with toasted bread and baked chicken.
- Snacks: Hard-boiled egg with pears canned in juice or water; raspberries and lactose-free plain yogurt.
3: Taking Dairy Alternatives and Plant-Based Delights
- Breakfast: Sweet potato toast topped with scrambled eggs and cheddar cheese. Add a banana.
- Lunch: Tuna salad made with lactose-free, nonfat Greek yogurt and hard-boiled egg, served on whole grain crackers or bread. Add applesauce sprinkled with cinnamon.
- Dinner: Salmon cakes served with mashed potatoes and roasted carrots, using olive oil for salmon cakes and carrots.
- Snacks: Overnight chia pudding with almond milk and cinnamon; banana with warmed peanut butter.
4: Balancing Fiber and Flavor
- Breakfast: A smoothie made with lactose-free milk or a dairy alternative like almond milk, a medium banana, two tablespoons of peanut or almond butter, unsweetened cocoa powder, and ground flaxseed.
- Lunch: Quinoa salad from pre-cooked and cooled quinoa with chopped cucumbers, tomatoes, bell peppers, feta cheese, and olives. The dressing consists of olive oil, lemon juice, basil, salt, and pepper. Add cooked chicken for extra protein.
- Dinner: Three-bean chili made with black beans, red kidney beans, pinto beans, diced tomatoes, garlic, and tomato paste, served with homemade cornbread.
- Snacks: Hummus and crackers; walnuts and pear applesauce.
5: Exploring Nutrient-Dense Options
- Breakfast: Bean-based muffins using navy beans added to a banana muffin recipe, paired with scrambled eggs, squeezed fruit, and vegetable juice.
- Lunch: Leftover three-bean chili served over a small baked potato, topped with shredded cheddar cheese if tolerated.
- Dinner: Baked cod, flounder, or salmon served with rice and cooked vegetables (green beans or zucchini), seasoned with olive oil, garlic, lemon juice, salt, and pepper.
- Snacks: Plain lactose-free nonfat yogurt; hard-boiled egg and crackers.
6: Comfort Foods with a Healthy Twist
- Breakfast: Energy bites made with old-fashioned oats, chia seeds, peanut butter, unsweetened cocoa powder, pure maple syrup, and mini dark chocolate chips paired with a small banana or raspberries.
- Lunch: A green smoothie made with avocado, lactose-free milk (or a dairy alternative), frozen banana, ground flaxseed, cannellini, or navy beans. Avoid high-insoluble fiber veggies if IBD is not well-managed.
- Dinner: One-pot slow cooker chicken with slow-cooked carrots and potatoes, seasoned with oregano, black pepper, salt, and parsley.
- Snacks: Baked apples and energy bites; Colby cheese and crackers.
7: Celebrating Culinary Diversity and Classic Favorites
- Breakfast: Microwaved old-fashioned oats with lactose-free milk, ground flaxseed, cinnamon, chopped walnuts, and cooked apples.
- Lunch: A grown-up charcuterie board with water-packed tuna, hummus, crackers, black and green olives, pears, or peaches canned in water or fruit juice.
- Dinner: Mashed potato bowls topped with tender slow-cooked chicken or turkey, served with cooked garlic, green beans, and baked pears.
- Snacks: Popsicles made from smoothie leftovers; peanut butter mixed into unsweetened Greek yogurt topped with dark chocolate chips (if tolerated).
Tips for Success
- Hydration: Drink plenty of water throughout the day.
- Avoid Trigger Foods: Spicy, high-fiber, and fried foods.
- Consultation: Always consult a healthcare provider or dietitian before making significant dietary changes.

Foods to Avoid With Ulcerative Colitis
Managing ulcerative colitis involves understanding which foods can trigger symptoms and cause flare-ups. While triggers vary from person to person, certain foods are problematic, especially during active UC symptoms.
Dairy Products: Dairy products can trigger symptoms if you’re lactose intolerant. Lactose intolerance is common among people with UC, so avoiding milk, cheese, and other dairy products may be necessary.
Inflammatory Foods: Certain foods can increase inflammation and should be avoided. These include processed meats (like bacon, sausage, and hot dogs), red fatty meats, and high-fat meats.
Alcohol and Caffeine: Both alcohol and caffeine can irritate the digestive system. Limiting or avoiding these beverages can help manage UC symptoms.
Spicy Foods and Hot Sauces can irritate and exacerbate symptoms during a flare-up.
Carbonated Beverages and Sorbitol: Carbonated drinks and products containing sorbitol (like sugar-free gum and candies) can cause gas and bloating, leading to discomfort.
Sugary and Processed Foods: High-sugar foods and beverages and processed foods low in vitamins and minerals can trigger symptoms. This includes candies, chips, frozen dinners, and other highly processed snacks.
Preparation Tips: Opt for cooked vegetables and fruits, as cooking makes them easier to digest. Canned vegetables and fruits, which are often peeled and cooked, are also good options. Reducing the size and coarseness of insoluble fiber by chopping foods into small pieces or incorporating them into smoothies and soups can help prevent irritation.
Remember: what works for one person may not work for another. Consulting with a registered dietitian can help tailor a diet plan that suits your needs and helps manage your UC symptoms.

Conclusion
If you have ulcerative colitis, you need careful dietary planning to manage your symptoms. This 7-day meal plan for ulcerative colitis offers a balanced approach, incorporating anti-inflammatory foods that are gentle on the digestive system.
Individuals with UC can better control flare-ups by focusing on easily digestible meals. Furthermore, avoid common trigger foods such as high-fiber, dairy, and processed foods. Personalization is key to managing UC—what works for one person may not work for another.
Meanwhile, you should consult a registered dietitian to get a diet plan for your specific needs. You must stay hydrated, avoid known triggers, and enjoy nutritious meals.
Other Resources
Crohn’s and Colitis UK, 2023.
How to Build a Meal Plan with Ulcerative Colitis (UC)
This article is for informational purposes only and does not substitute professional medical advice. Consult a qualified healthcare provider for personalized guidance.